In May 2018, the government announced a far-reaching review of New Zealand's health and disability services, with a view to identifying potential changes to improve the sector's performance, structure and sustainability while also achieving equity of outcomes for Māori and Pacific peoples.1
Terms of reference were released in August 2018, and an expert review Panel (the Panel) was established, chaired by Heather Simpson. An interim report followed in September 2019. While the final report was completed in March 2020, the Minister of Health declined to accept it due to the COVID-19 lockdown, preventing its publication.2
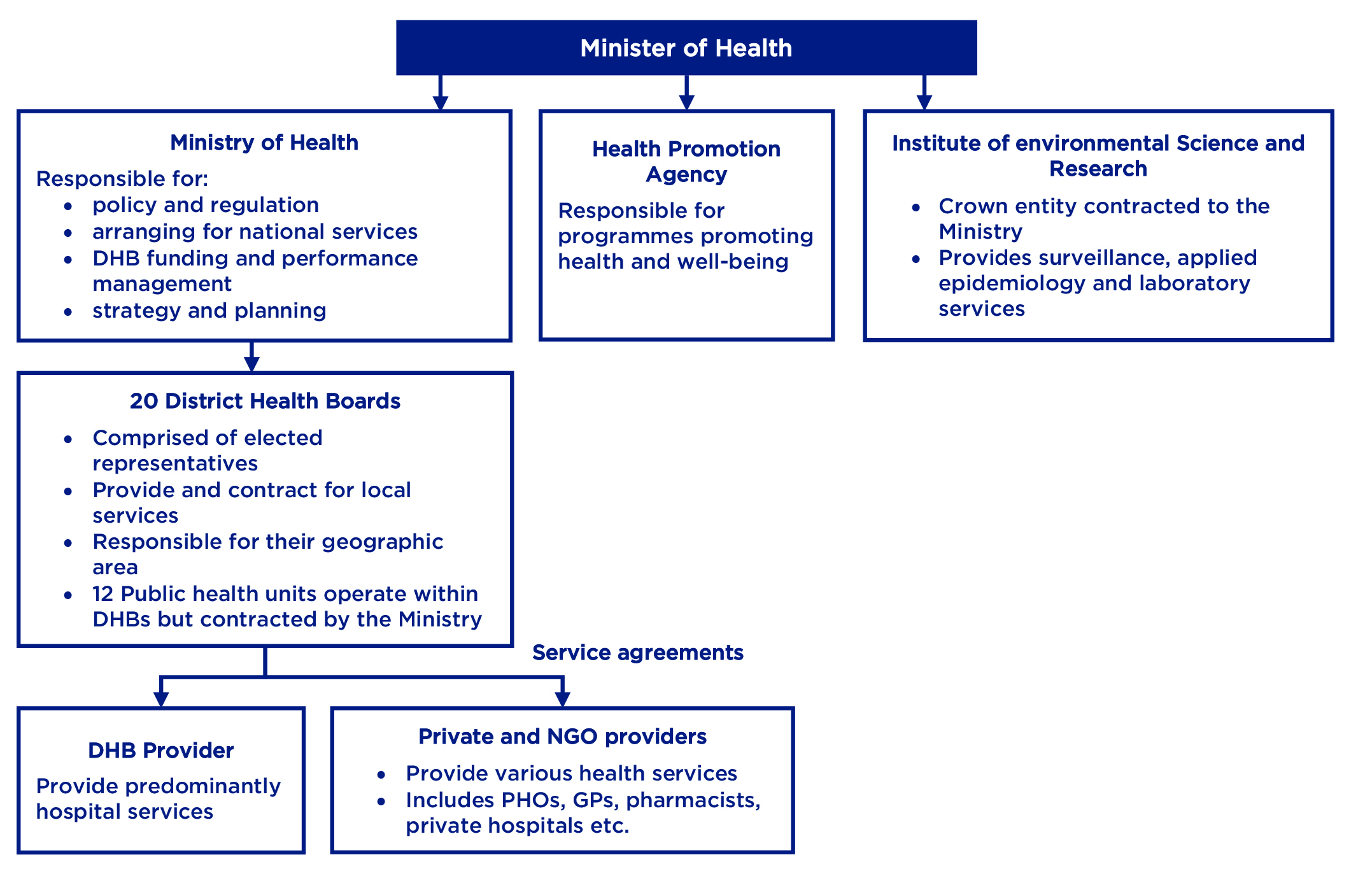
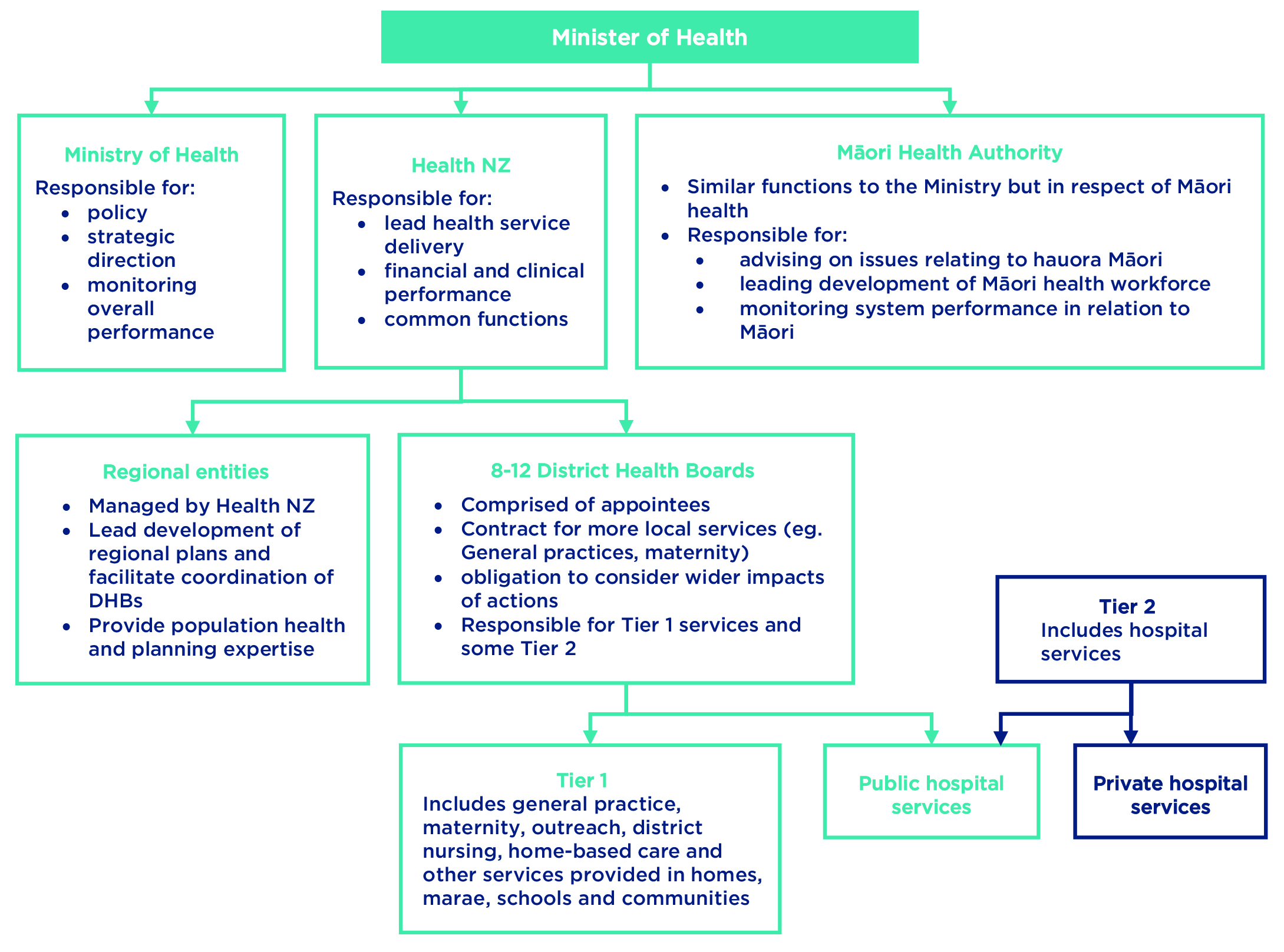
That report has now been released. In opening, the Panel acknowledge that New Zealand has a very good publicly funded health system by global standards. However, it faces a number of challenges, including increasing demand (including as the population ages) and limited financial resources.3 In particular, poorer health outcomes were generally observed for Māori and Pacific peoples, as well as disabled people and those living in rural communities.4 In response, the Panel has recommended sweeping changes that would significantly alter the sector as we know it. The diagram below highlights the impact the recommendations would have on the structure of the health and disability sector.
Current model
Proposed model
Below we consider some of the main changes recommended by the review.
New health authorities
The review concluded that “more active leadership" and greater cohesion was required at all levels throughout the system.5 To assist with this, the Panel proposed a new Crown entity, referred to as Health NZ.6
Under the Panel's proposals, Health NZ would be responsible for leading health service delivery, both in terms of clinical and financial outcomes. The new agency would be accountable to the Minister of Health.7 While the Ministry of Health's role would be streamlined to focus on monitoring overall performance, policy and strategic direction, Health NZ would become responsible for financial performance, undertaking common functions (e.g. back office functions) to increase cost savings and working towards clinical improvement.8 It would also be responsible for developing a long-term investment plan for facilities and digital technology.9
In terms of the new body's structure, to reflect the principles of Te Tiriti o Waitangi, the Panel proposed that Health NZ's Board be comprised of equal numbers of Crown and Māori representatives.10 The review further recommended that legislation provide for a charter for Health NZ, to clearly outline the culture and behaviours expected of the health workforce.11 This charter should recognise the importance of reflecting diversity and maintaining relationships with Māori as tāngata whenua.
In addition, the Panel recommended that a new Māori Health Authority be established to sit alongside Health NZ. This body would act as a partner for the Ministry of Health, having similar functions in respect of Māori health as the Ministry of Health does generally. It would operate as an independent departmental agency, directly accountable to the Minister.12 This body would provide advice on issues relating to hauora Māori, while also leading development of the Māori health workforce and increases in the range of kaupapa Māori services.13 Beyond this, the Māori Health Authority would monitor the health system's performance in relation to Māori, identify issues and then look to develop solutions.14 It would also assist in developing policy to embed mātauranga Māori practices throughout the health and disability system.15
One matter which would need to be determined is the extent to which the Māori Health Authority should control funding for services for Māori. While the Panel was otherwise generally in agreement, its report indicates that it was unable to reach a consensus on this particular point.16
Changes to the DHBs
The review also recommended a number of structural changes to the current District Health Boards (DHBs). In particular:
- The Panel proposed reducing the current 20 DHBs down to between eight and 12 within the next five years.17 This process would be led by Health NZ and form part of a wider process of moving towards regional collaboration.18
- The Panel also found that the arguments for retaining elected members were “not compelling",19 referencing elected boards' “blurred accountabilities" and the declining number of voters participating in DHB elections.20 Instead, it proposed that members of DHBs be appointed directly by the Minister. A set of competencies would be developed for such appointees, to ensure that they had appropriate knowledge of finance, governance, tikanga Māori and issues specific to the health and disability sector.21
- The Panel recommended that the scope of DHBs' considerations should be broadened, noting that, at present, DHBs are responsible only for what happens within their particular geographic area. The Panel proposed that instead DHBs should be required to consider how their services impact the system as a whole.22 They would also be required to collaborate in producing Regional Strategic Plans as part of the move towards greater regional collaboration,23 while regional entities managed by Health NZ would be established to facilitate that collaboration.24
- The Panel further recommended changes to the way in which DHBs are funded. Specifically, it proposed that ethnicity and socioeconomic deprivation be given greater weighting when calculating funding, as well as more comprehensive requirements for DHBs to disclose and report against their indicative budgets.25
Such changes would represent a major shift in approach, retaining a focus on local communities, but ultimately moving towards a more centralised model overseen by Health NZ.
Further recommendations
The Panel also recommended:
- the principles of Te Tiriti o Waitangi be added to key health legislation, which is consistent with the recommendations of the Waitangi Tribunal's Hauora Report (Wai 2575);26
- a clear New Zealand Health Plan be developed, spanning a timeframe of 10 to 15 years, to guide the long-term strategic direction of the sector.27 DHBs would then produce district strategic plans covering the next five to 10 years;28
- reduced reliance on national contracts for some services e.g. for general practice services and similar;29 Instead, local planning processes would result in localities being served by a network of publicly funded services, with some services common nationwide and others tailored to the specific needs of local populations.30 New contract terms should have a strong emphasis on enabling connected and whanau-centred service delivery;31
- a move towards other services being nationally commissioned, where such consistency is desirable and economies of scale can be achieved, with potentially joint purchasing between DHBs/Health NZ and ACC.32 In developing a commissioning policy, consideration should be given to whether procurement rules and guidance allow for sufficiently equity and population-focused practices.33 The Panel further recommended greater transparency in terms of the framework for planning and investment decisions;34
- increasing the Ministry of Health's population health expertise;35
- providing for guaranteed increases to Vote Health to help maintain the system's overall quality.36 In addition, it recommended additional funding to “rebalance" the system and address deficits, with this funding to be allocated to Health NZ initially to be apportioned across DHBs;37and
- the Ministry work with the Tertiary Education Commission, Health NZ and the new New Zealand Institute of Skills and Technology to ensure that training for healthcare workers is consistent and to develop more “learn as you earn" options and shorter cumulative programmes.38
The Government's response
The Government has indicated that it is committed to long-term reform of the health and disability system in line with the report's recommendations. In a statement, the Minister of Health said that Cabinet had accepted “the direction of travel" outlined by the Panel, including changes to “reduce fragmentation", improve leadership, accountability and equity.39
To that end, the government has indicated that it will form a group of Ministers (including the Prime Minister, Minister of Finance and the Minister and Associate Minister of Health) to drive changes. In addition, the Health Minister will establish a Ministerial Committee under s 11 of the Public Health and Disability Act 2000 to provide advice, while an implementation team led by the Department of Prime Minister and Cabinet will be responsible for policy and design.40
Conclusion
The recommendations put forward by the review Panel are far-reaching and have significant implications for a number of organisations in the sector. Reform of this scale is likely to take some considerable time; however, it will be important for parties involved in the health and disability sector to participate in the reform processes as they develop and be ready to adapt to change when the time comes.
If you have any questions about the matters raised in this article, please get in touch with the contacts listed, or your usual Bell Gully adviser.
If you wish to receive further health updates you can sign up here.
1 Final Terms of Reference – Review of New Zealand Health and Disability System. The review did not encompass ACC, PHARMAC or private health insurance.2 Carmen Parahi “Government fends off major health system review to avoid distraction from COVID-19" Stuff (2 April 2020).
3 Health and Disability System Review: Final Report (March 2020) at 3.4 Health and Disability System Review: Final Report (March 2020) at 21.5 Health and Disability System Review: Final Report (March 2020) at 5, 42.6 Health and Disability System Review: Final Report (March 2020) at 5.7 Health and Disability System Review: Final Report (March 2020) at 5.8 Health and Disability System Review: Final Report (March 2020) at 44, 61.9 Health and Disability System Review: Final Report (March 2020) at 250.10 Health and Disability System Review: Final Report (March 2020) at 6.11 Health and Disability System Review: Final Report (March 2020) at 48.12 Health and Disability System Review: Final Report (March 2020) at 26.13 Health and Disability System Review: Final Report (March 2020) at 26.14 Health and Disability System Review: Final Report (March 2020) at 6.15 Health and Disability System Review: Final Report (March 2020) at 30.16 Health and Disability System Review: Final Report (March 2020) at 2.17 Health and Disability System Review: Final Report (March 2020) at 5.18 Health and Disability System Review: Final Report (March 2020) at 46-47.19 Health and Disability System Review: Final Report (March 2020) at 5.20 Health and Disability System Review: Final Report (March 2020) at 49.21 Health and Disability System Review: Final Report (March 2020) at 5.22 Health and Disability System Review: Final Report (March 2020) at 6, 46.23 Health and Disability System Review: Final Report (March 2020) at 46.24 Health and Disability System Review: Final Report (March 2020) at 244.25 Health and Disability System Review: Final Report (March 2020) at 7.26 Health and Disability System Review: Final Report (March 2020) at 6.27 Health and Disability System Review: Final Report (March 2020) at 55.28 Health and Disability System Review: Final Report (March 2020) at 56.29 Health and Disability System Review: Final Report (March 2020) at 8.30 Health and Disability System Review: Final Report (March 2020) at 103.31 Health and Disability System Review: Final Report (March 2020) at 108.32 Health and Disability System Review: Final Report (March 2020) at 74.33 Health and Disability System Review: Final Report (March 2020) at 76.34 Health and Disability System Review: Final Report (March 2020) at 78.35 Health and Disability System Review: Final Report (March 2020) at 45.36 Health and Disability System Review: Final Report (March 2020) at 58.37 Health and Disability System Review: Final Report (March 2020) at 62.38 Health and Disability System Review: Final Report (March 2020) at 248-249.39 Hon Dr David Clark “Building a stronger health and disability system" (16 June 2020).40 Hon Dr David Clark “Building a stronger health and disability system" (16 June 2020).
Disclaimer
This publication is necessarily brief and general in nature. You should seek professional advice before taking any action in relation to the matters dealt with in this publication.


