The reforms will have a significant impact on organisations and stakeholders within the health sector. In this article, we consider key aspects of the reform.
In June 2020, the Health and Disability System Review (the Review) was released, recommending sweeping changes to New Zealand's health sector. It identified that New Zealand's publicly funded health system faces a number of challenges, including increasing demand, limited financial resources, and inequity of health outcomes, particularly for Māori. We discussed some of the Review's key recommendations in a previous article.
Following consideration of the Review, Cabinet established The Health and Disability Review Transition Unit in September 2020 to lead the Government's response. On Wednesday, Minster of Health Hon Andrew Little and Associate Minister of Health (Māori) Hon Peeni Henare announced an extensive overhaul of the health and disability system. While the Review's recommendations and concerns for greater equity have largely been adopted, the Government has gone further. The diagram below highlights the structural changes.
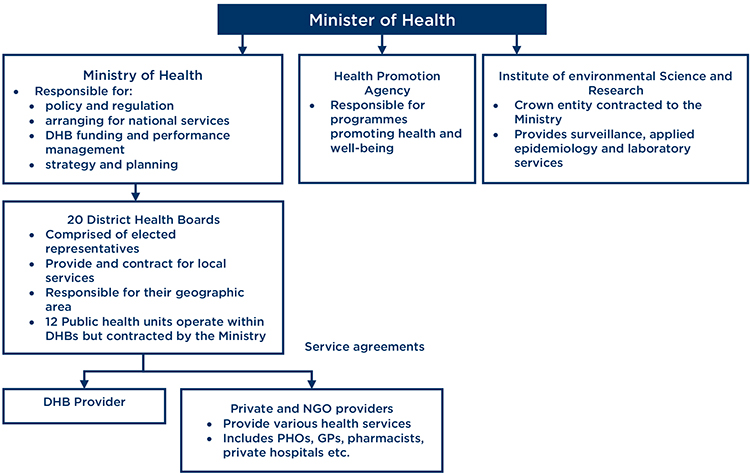
Current model
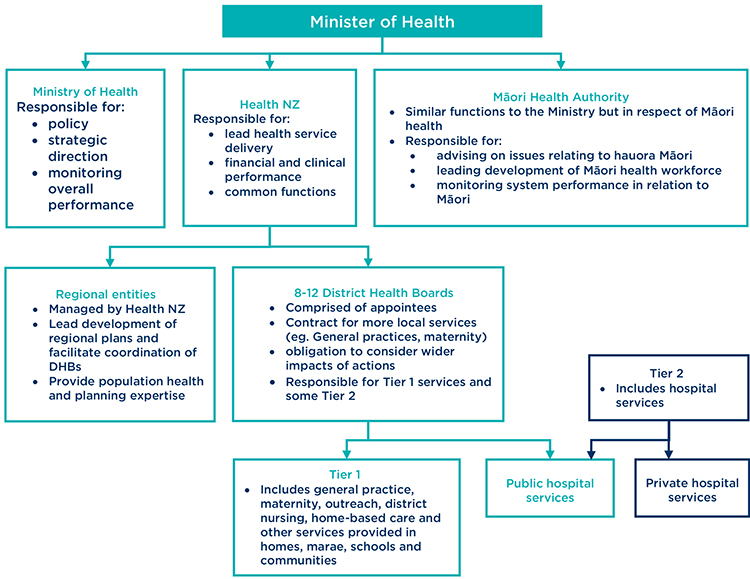
Model proposed by the Review
Model now proposed
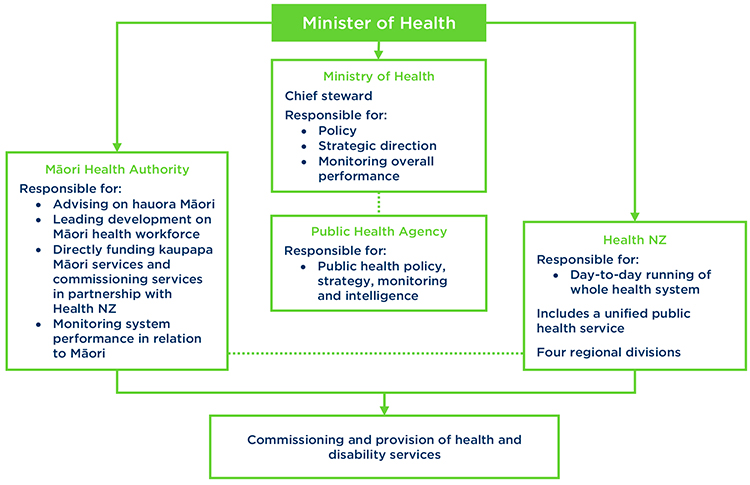
Below, we consider some of the main changes to the system now proposed by the Government.
Health New Zealand – a Crown entity to replace the DHBs
A new Crown entity, Health New Zealand (Health NZ), will replace the 20 existing District Health Boards (DHBs) to centralise New Zealand's health system. Health NZ will be responsible for planning, commissioning, delivering and managing all health services for the entire population.1 It will also take on the operational functions of the Ministry of Health, such as managing national contracts. Four regional divisions of Health NZ will be responsible for commissioning primary and community services e.g. for general practice services.2 This will be facilitated through locality plans, which set the priorities of particular communities.3 Each of the four regional divisions will also oversee and manage a network of hospitals. It is not yet clear how those regions will be structured.
Health NZ will include a national public health service, which will consolidate the existing 12 Public Health Units into one service, in order to better coordinate service (e.g. responses to threats such as COVID-19).
Māori Health Authority
A Māori Health Authority (yet to be named) will sit alongside the Ministry of Health and Health NZ. It will be the principal advisor on hauora Māori and will monitor and report to the Minister of Health on the performance of the health and disability system in relation to Māori health outcomes.4 It will also work in partnership with Health NZ to commission care across New Zealand and to directly fund some health services targeted at Māori, including more kaupapa Māori services.5 This funding power is a departure from the Review, which had not concluded on the extent the Māori Health Authority should control funding. In addition, the Māori Health Authority will work with Iwi-Māori Partnership Boards, Māori health providers and Māori communities to understand Māori health needs across New Zealand, with the aim of building a stronger Māori workforce and provider network. The rationale for these reforms is the poorer health outcomes for Māori seen over past decades, with the Government noting in its White Paper Summary that “these inequities cannot continue".6
The Government will work with Māori on the specific design of the Māori Health Authority. An interim Māori Health Authority will be established as a departmental agency by the end of 2021.
The Ministry of Health
The Ministry of Health will no longer directly fund and commission health services. Its role will be streamlined to focus on monitoring overall performance, policy and strategic direction. The Ministry will remain “chief steward" for the health and disability system, meaning it will remain in charge of ensuring all parts of the system are working cohesively to deliver care.7
Public health
In response to the Review's calls for increased population health expertise within the Ministry, a new Public Health Agency will sit within the Ministry of Health and will be responsible for public health policy, strategy, monitoring and intelligence.8 This means public health will now be operated nationally.
Although reform was initiated prior to the COVID-19 pandemic, coordination of public health policy may be of particular benefit to New Zealand's ongoing response to the pandemic – especially given comments made by the Office of the Prime Minister and Office of the Minister of Heath in a paper to Cabinet that COVID-19 “reinforced the importance of population (or public) health".9 The Health and Disability Review Transition Unit have also noted that COVID-19 highlighted the 12 current Public Health Units “needed better national coordination and leadership when responding to nationwide threats, and to be able to better spread best practice and improvements across the system".10
From review to reform
The most significant departure from the recommendations made by the Review is the decision on DHBs. The Review recommended that Health NZ be established, but did not go as far as to suggest it be empowered to deliver or commission care. Given the Review instead recommended a reduction in DHBs to between eight and 12 within the next five years,11 the Government's decision to disestablish DHBs altogether may have come as a surprise to many. However, the Review was critical of the DHB structure, including the election of members,12 the scope of DHBs, and the way they are currently funded.13 It recommended that DHBs “operate as part of a cohesive system"14 and produce Regional Strategic Plans as part of a move towards greater regional collaboration.15 In this sense, the Review was in favour of New Zealand moving towards a more centralised and collaborative healthcare model. The Government has adopted a collaborative model largely along the Review's lines, but has determined that Health NZ will be best placed to administer this, rather than a smaller number of DHBs.
Where to from here?
The Government has indicated that the formal date for the new structure is likely to be July 2022. At this time, all DHB staff will transfer to Health NZ.16 For now, the first 18 months will be a preparation and transition phase. Towards the end of 2021, interim entities with acting chief executives will be established to plan and build capability for the future system.17 Legislation must then be passed to establish the various health authorities as formal organisations, including Health NZ as a Crown entity. The focus will then turn to an expansion and development phase, “which will see the new system become more established and embed and refine new ways of working".18
There are further decisions to be made by Cabinet. The Review recommended that the Board of Health NZ be comprised equally of Crown and Māori representatives.19 There has been no comment as of yet on the Government's response to this recommendation. In addition, there has been little word on whether legislation will be amended to incorporate Te Tiriti o Waitangi principles across the system as per the Review's recommendation.20 The Government has indicated that further announcements are to come, including on funding, workforce and digital health.21
The proposed reform of our health and disability system will be extensive. There will be further design work in relation to the new arrangements over the coming months. Organisations within the health sector and other stakeholders should remain attuned to these changes and take any opportunities that may arise within the coming months to engage with the process.
If you have any questions about the matters raised in this article please get in touch with the contacts listed or your usual Bell Gully adviser.
1 DPMC “Fact sheet: Stewardship" (April 2021).2 DPMC “Fact sheet: Health New Zealand" (April 2021).3 DPMC “Fact sheet: Primary and community care" (April 2021).4 DPMC “Fact sheet: Hauora Māori" (April 2021).5 DPMC “Health Reform: White Paper Summary" (April 2021).6 DPMC “Health Reform: White Paper Summary" (April 2021).7 DPMC “Fact sheet: Stewardship" (April 2021).8 DPMC “Fact sheet: Public Health" (April 2021).9 Cabinet Paper “Response to the Health and Disability System Review / Haora Manaaki Ki Aotearoa Whanui" CAB-20-SUB-0269 (30 November 2020) at [10].10 DPMC “Fact sheet: Public Health" (April 2021).11 Health and Disability System Review: Final Report (March 2020) at 47.12 Health and Disability System Review: Final Report (March 2020) at 49.13 Health and Disability System Review: Final Report (March 2020) at 64.14 Health and Disability System Review: Final Report (March 2020) at 63.15 Health and Disability System Review: Final Report (March 2020) at 46.16 DPMC “Fact sheet: Implementation Roadmap" (April 2021).17 DPMC “Fact sheet: Implementation Roadmap" (April 2021).18 DPMC “Fact sheet: Implementation Roadmap" (April 2021).19 Bell Gully “Health and Disability System Review – a new prescription" (19 June 2020).20 Health and Disability System Review: Final Report (March 2020) at 6.21 DPMC “Health Reform: White Paper Summary" (April 2021).
Disclaimer
This publication is necessarily brief and general in nature. You should seek professional advice before taking any action in relation to the matters dealt with in this publication.


